The Blesser’s Curse
Olga Khazan,
The Atlantic, Mar 22, 2018
daddies and vaginal microbes created the world’s largest HIV epidemic

South Africa—Mbali N. was just 17 when a well-dressed man in his 30s spotted
her. She was at a mall in a nearby town, alone, when he called out. He might
have been captivated by her almond eyes and soaring cheekbones. Or he might
have just seen her for what she was: young and poor.
to ignore him, she told me, but he followed her. They exchanged numbers. By the
time she got home, he had called her. He said he wasn’t married, and she
doesn’t know if that was true. They met at a house in a different township; she
doesn’t know if it belonged to him. Mbali, who is now 24, also doesn’t know if
he had HIV.
enjoyed spending time with the man during the day, when they would talk and go
to the movies. But she didn’t like it when he called at night and demanded to
have sex, which happened about six times a month. When she refused him, he beat
her. For her trouble, he gave her a cellphone, sweets, and chocolates.
time, she had another boyfriend, who was her own age. The older man ordered her
to leave the younger boy, and when she refused, he beat her again. Eventually,
she grew tired of the abuse and ended the relationship.
Mbali lives with her grandmother in Vulindlela, a verdant rural area near the
eastern coast of South Africa, in the humid, hilly province of KwaZulu-Natal.
Vulindlela means “open a way”
in Zulu, but like many young women here, Mbali faces a lot of closed doors. She
graduated high school but didn’t have the money for college, so she spends most
of her days helping her grandmother with housework and taking care of her
2-year-old son. I asked if her experience with her “blesser,” as men who
initiate transactional relationships are known here, prompted her to warn her
friends against dating older men. She let out an exasperated little laugh.
said. “They’ll just say I’m so jealous.”
HIV negative. But 36 percent of the adults in Vulindlela are positive, as are
about 60 percent of the women aged 25 to 40. Although HIV infection rates have
stabilized globally, hundreds of thousands of South Africans are infected
every year; more than 7 million live with the virus in their bodies. And in the
midst of this, the largest HIV epidemic in the world, the HIV prevalence among
adolescent girls is roughly five times greater than that of boys. By performing
genetic analyses on samples of HIV virus in Vulindlela, researchers have
concluded that the high rate of infections here—among both sexes—is driven in
part by relationships like the one Mbali had when she was 17.
country where two-thirds of people under age 25
are unemployed, some poor South African women and teens date older,
wealthier men, who provide them with everything from food to hairpieces to
school uniforms. In exchange, the men demand discreet, often condom-free sex.
At the same time, many of these young women maintain more egalitarian relationships
with boys their own age. Some of the sugar daddies, as these men are also
sometimes called, infect the girls with HIV. When those teen girls reach
adulthood, they find husbands and pass their HIV onto them. Those husbands, in
turn, become the next crop of sugar daddies, infecting the next generation of
teen girls and perpetuating the cycle.
cycle of contagion, researchers are finding, is driven not only by economics
and culture but also by the human body’s own microbes. The reproductive tract
is home to a delicate balance of bacteria, some of which appear to keep HIV and
other viruses at bay. The grooming practices some South African women use to
entice wealthy boyfriends might be upsetting this balance, and increasing their
risk of HIV infection.
Abdool Karim, the epidemiology professor who is uncovering these connections,
has a gray beard and enormous voice. When he was a student, everyone called him
Slim, Afrikaans for “clever,” and the name has stuck. He’s of Indian descent,
which meant that, under the country’s apartheid-era racial code, he was
funneled into the country’s only medical school for nonwhites at the University
of Natal, now known as the University of KwaZulu-Natal, in Durban. It’s where
he’s worked off and on for more than three decades, and it’s where he and his
wife, the epidemiologist Quarraisha Abdool Karim, run the Center for the AIDS
Program of Research in South Africa, or CAPRISA. They spend their days trying
to figure out why, exactly, South Africans keep dying of a disease that much of
the world has nearly forgotten.
early ’80s, HIV was still relatively unknown in South Africa. Salim only
realized the awful extent of the disease in 1987, when he moved to New York to
study public health at Columbia University. It was a terrifying time: Around half a
million people in the city had the virus, which was poorly
understood. A prostitute who bit a policeman and claimed she had AIDS was walked
into the courtroom by officers wearing surgical masks. “You couldn’t escape HIV
in New York,” Salim told me in his office one day in February. In New York, it
became clear to the Abdool Karims that HIV was about to ravage southern Africa.
Quarraisha returned to Durban and zoomed in on a puzzling trend: While many in
the United States still viewed HIV as a gay men’s disease, the South Africans
with HIV were disproportionately young, heterosexual, and female. Though the
disease was still relatively rare, girls were getting HIV five to seven years
younger than their male counterparts. That, the Abdool Karims realized, meant
young mothers would pass the infection onto their kids. A whole generation of
nurses and teachers—the jobs dominated by women—might be wiped out. “Oh, my
goodness,” Salim thought. “This is a tragedy on a scale that we have yet to
even grapple with.”
“Girls
here are happy to have a boyfriend from Johannesburg to take them out of
poverty.”
kills more than 100,000 South Africans—roughly the population of
Green Bay, Wisconsin—each year. While antiretroviral drugs, widely available
for free in South Africa, can halt HIV’s erosion of the immune system, there
are simply too many South Africans with too high a risk of getting HIV for the
country to treat its way out of the problem. Everyone seems to agree:
Prevention is key.
’90s, the Abdool Karims began studying different substances that had the
potential to prevent HIV infection, especially in women. For the most part,
they were a bust: When they tested nonoxynol-9, a spermicide, in a small group
of truck-stop sex workers, not only did it have no effect on infection rates,
but the substance also inflamed the women’s vaginas, causing burning and
itching.
progress improved in 2003, when they began testing a drug called tenofovir,
which prevents the virus from replicating and seemed to have few side effects.
In 2010, Quarraisha presented the findings of their tenofovir gel study at the
International AIDS Conference in Vienna: When women applied the gel to their
vaginas before and after sex, she reported, the risk of HIV infection dropped by 39 percent.
For the first time, women had a way to reduce their risk of HIV infection that
didn’t require their partners’ permission. It was a rare glimmer of hope in
what had become a dismal field, and the conference attendees rewarded
Quarraisha with a standing ovation.
Abdool Karims were elated and proud. But still, they wondered: Why only 39
percent?
Vulindlela, women walk alongside dirt roads with babies slung on their backs,
and people still answer to the three local amakhosi, or Zulu chiefs. Older
people smear red clay on their skin to protect it from the sun. Horses and cows
roam the streets freely, and outhouses dot the rolling hills. Today, most
people live in small, cinder-block houses, but when CAPRISA first began doing
research here in 2001, many still dwelled in traditional mud huts.
late 1800s, in KwaZulu-Natal and several other areas, the colonial government
imposed a tax on every hut “occupied by a native.” They exempted
“houses of European construction” occupied by residents “conforming to
civilized usage.” The tax burden forced many Zulus to work in the gold mines,
some of which were hundreds of miles away. Miners usually lived in single-sex
hostels for much of the year, returning to see their families only every few
months. Separated from their wives, the men turned to sex workers, who became
vectors of sexually transmitted diseases.
want to create a society in which you wanted a sexually transmitted infection
to spread,” Salim said, “you couldn’t do it better than the way in which the
colonialists designed South Africa. They designed it to create family
instability.”
 |
|
A woman
sits inside her house in Vulindlela, South Africa.
(Khaya Ngwenya / The
Atlantic) |
Though
the situation is less extreme now that apartheid has ended, itinerant labor
remains common, and many men maintain multiple
partners. Men who are able to get good jobs are sought after as
patrons and partners by women who aren’t.
his colleagues wanted to pinpoint exactly who was getting HIV in KwaZulu-Natal,
and from whom. In 2014, CAPRISA staff collected blood from the residents of
nearly 10,000 households in Vulindlela. They looked at the HIV viruses inside
the samples and analyzed each virus’s genes. They identified clusters in which
people had passed the virus to one another.
found that the girls in their teens and early 20s were getting infected by men
who were, on average, about nine years older than they were. When they reached
their late 20s, these women were infecting partners of their own age, who often
didn’t realize it right away. With wandering eyes and high levels of the virus
coursing through their blood, some of the men were then infecting the next crop
of 16- and 17-year-old girls.
percent of the men who were passing HIV to younger women had older, female
partners at the same time. I wondered aloud to Salim how a society could become
so overrun by sugar daddies when the consequences—for women and men—are so
severe. What he guessed was this: In many cases, the girls’ parents know about
the blessers. “Many of them also support the girl’s family,” he said.
Mahlase, a community leader in Vulindlela, told me that the poverty here used
to be much worse, and the effects were often fatal. Under apartheid, the
country’s rural areas had little infrastructure, and the sick had to be carried
to the hospital. In the 1980s and ’90s, some women Mahlase knew had 16 children.
They frequently died in childbirth from conditions like high blood pressure,
which women in more affluent nations can typically survive with access to
medical care.
conditions have improved somewhat, but many people here and across South Africa
are still sorely in need of jobs. Among the legacies of apartheid is one of the
highest levels of income inequality on earth. On the beach in Durban, the
largest city in KwaZulu-Natal, I saw a thin man pick a plastic bag out of a
garbage can and lick off its residue—right next to a watchtower advertising the
area as the Bay of Plenty. Many kids have no choice but to attend high schools
where 60 students might cram into a classroom. Poor and middle-class families
often don’t have the means to pay for college and can’t get loans.
here are happy to have a boyfriend from Johannesburg to take them out of
poverty,” Pamela Gumbi, a scientist at the Vulindlela CAPRISA clinic, told me.
In the Valley of a Thousand Hills, a community not far from Vulindlela that
looks exactly like its bucolic-sounding name, high schoolers told me local
girls were dating the region’s big earners: the drivers of minibus taxis.
 |
|
A woman
walks in the Valley of a Thousand Hills.
(Khaya Ngwenya / The Atlantic)
|
blesser trend shapes men’s lives, too. In a village north of Vulindlela called
KwaMsane, I talked with a group of men who were hanging out by a
shipping-container snack store in the middle of the day, eating sugarcane as
chickens pecked at the grass nearby. A 33-year-old named Zothani bemoaned the
lack of local job opportunities, suggesting that leads to some of the sexual
practices researchers and policy makers are trying so desperately to change.
“The more time we are not working, the more people are giving birth, giving
birth,” he said.
young men told me that they worry girls won’t want to date them unless they are
able to buy them things—a modern anxiety layered on top of the Zulu custom of lobola,
in which suitors pay a bride price of several head of cattle.
said they don’t mind if their girlfriends have sugar daddies; they think they
stand to benefit. “I’m unemployed, so if she has an extra relationship, that
money supports me,” said Sanele Ndlovu, a 20-year-old construction worker in
Vulindlela, who was speaking hypothetically.
few other men I talked to, Ndlovu is even starting to think he should try to
find a sugar mama. The women are doing it, so why not? “There’s nothing wrong
with falling in love with an older woman,” he said. “She’s cute, she has no
husband, so capitalize on the opportunity.”
soon as the sugar-daddy trend became widely known in South Africa, it became
oversimplified in the media and in popular imagination. There’s a perception,
among some here, that the women who seek out sugar daddies are vain and
irresponsible. They want nice weaves—considered more fashionable than
close-cropped natural hair—and clothes that will look stylish on Instagram, the
thinking goes. That makes it easy to blame women for the consequences of
promiscuity. “You take a decision to say, ‘I will take off my clothes’—you just
can never say it was a mistake,” said the KwaZulu-Natal health minister, Sibongiseni
Dhlomo, addressing a tent full of schoolkids in 2016. “Let there be
no one who will say they don’t know what happened when they fall pregnant …
Therefore, it is up to you to ensure that does not happen.”
stereotypes are reinforced by the rise of websites like BlesserFinder, which
tries to connect sugar daddies with those hoping to be “blessed.”
(BlesserFinder was started by a man,
according to news reports.)
conversations with women who have had transactional sex, or who know those who
have, revealed a more complicated picture. For one thing, the women who have
blessers aren’t very promiscuous. In CAPRISA’s Vulindlela study, most people
had fewer than five sex partners in their lifetimes. The average American Baby
Boomer, by comparison, has had 11.
sex they are having is very risky. Many of the sugar daddies refuse to wear
condoms, saying they “don’t want to waste their money on plastic,” as one
teenager put it to me. Women avoid disclosing their HIV statuses to their sugar
daddies out of fear they’ll be cut off financially. Since many of the sugar
daddies are married, young women meet them at hotels and don’t tell their
parents where they are, heightening their vulnerability to violence. In
Pretoria, a 15-year-old was recently found dead
in a pit latrine after telling her friends she had gone to meet an older man.
The suspect, a 33-year-old man, had posted on Facebook that he wanted to find a
curvy woman to bless.
“We are
Zulus. We don’t talk about sex.”
The idea
that women who have blessers are making bad choices also presumes that there
are better choices available. I met A., a pretty, dark-skinned 31-year-old, in
a cold, dark exam room of a clinic in Durban. She lives in Umlazi, a large
township nearby. She calls it a place for “poor people,” with too many tsotsis—criminals.
baby at 16 and dropped out of high school. She and the baby’s father broke up
because he beat her, she says, pointing to scars on her arms. She now has HIV,
and when her mother found out she almost made her go to an inyanga, a
traditional healer. She says no one ever told her about condoms. “We are Zulus.
We don’t talk about sex,” was the attitude at home, she said.
unemployed. For food, cellphone minutes, and things for her daughter, she turns
to a new, older man she’s dating, who she says “treats me well sometimes.” He’s
married, and she feels bad when his wife calls to chew her out. “I’m dating
this married guy because I get whatever I want,” she says. Meanwhile, she’s
also dating a “poor guy, because he’s the love of my life.”
looking for a job as a housekeeper—a profession she likes because sometimes,
her employers feed her. “Other jobs you have to bring your own food,” she said,
“which is not gonna happen because sometimes we have just sleeping food, and in
the morning there’s no food.”
the older man, the blesser, don’t use condoms, and she hasn’t told him that
she’s HIV positive. Mostly, she’s just hoping to start making her own money
soon. “Life is not good for someone who is not employed,” she said. “You sleep,
watch TV, sleep, watch TV.”
she added, “I don’t live my life.”
her eyes welled up with tears. A nurse standing nearby told me to stop my line
of questioning.
from Vulindlela, closer to the border with Swaziland, there’s a poor, sleepy
town called Mtubatuba. The most happening place to be is a club called the
White House, a small cement building with a large outdoor patio. On a recent
warm Friday night, a DJ spun Zulu dance music while groups of men and women
stood around tables, drinking, dancing in place, and taking selfies.
have been college night anywhere on earth. The bouncer told me many girls here
come with nothing and expect guys to buy them drinks all night. The girls might
go home with the best-looking or most generous of their benefactors. But this,
a practice familiar the world over, is not exactly “blessing.”
approached two 25-year-olds, Nkundu Matha and Thandeka Mathamulo, to ask if women
look for blessers here. No, they said, the guys are mainly locals, without
blesser-level jobs. If they did meet a blesser, I wondered, how would they
react if he asked them to have sex without a condom? “Nice to see you and
goodbye,” Mathamulo said.
attitude might help explain the results of a 2014 study
of the area by scientists from Harvard University and the Africa Health
Research Institute, who found no evidence that having an older male partner
increased the risk of HIV infection.
though the blesser phenomenon is real, it seems its effects are uneven, and the
country’s HIV epidemic is shaped by other factors, too. Some of them,
researchers are finding, are hidden within the women themselves.
when the Abdool Karims got their standing ovation in Vienna, they were
nevertheless confounded by the fact that the tenofovir gel didn’t fully protect
the women from HIV. They decided to investigate whether there was something
about a woman’s biology that increases her risk of contracting the virus.
CAPRISA released a study in which it measured the cytokines—proteins that serve
as markers of inflammation—in the vaginas of 889 women. They found that women
who had more of these cytokines, and thus more inflammation, were three times
more likely to get HIV over a three-year period. But where was this
inflammation coming from? To find out, they sequenced the entire vaginal
microbiomes of 120 women.
1,300 species of bacteria naturally occur in the vagina. A healthy vagina is
dominated by a “good” germ called Lactobacillus, which, under a microscope,
looks like a fistful of rod-shaped Mike and Ikes. It scrubs the genital tract
with a mild acid and helps keep the “bad” bacteria to a minimum.
“The Gardnerella
is eating up all the tenofovir!”
hoping to dissuade their patients from douching, sometimes liken vaginas to
self-cleaning ovens. But really, they are more like gardens that—for the most
part, and in most women—weed themselves. Sometimes, though, they get overrun by
invasive, pernicious flora. And that is where the trouble begins.
bivia, it turned out, was the main source of the inflammation that leads to HIV
infection. Prevotella is normally found in the gut, but it can migrate into the
vagina from the anus. In small numbers, it can be fine. But it can also swarm
the place, usurping the Lactobacillus and other healthy bacteria like
dandelions taking over a rose garden. On Prevotella’s surface are
lipopolysaccharides, which break off and spark inflammation. If a woman happens
to get exposed to HIV during a Prevotella inflammation, her risk of infection
is much higher.
scientists decided to test another “bad” bacterium, Gardnerella vaginalis,
typically associated with bacterial vaginosis, to see if it had an effect on
tenofovir. (Bacterial vaginosis, as many women know, can resemble a yeast
infection but must be treated with antibiotics.) Salim’s colleagues added tenofovir
to a culture of Gardnerella. Within four hours, about half the tenofovir was gone.
doing these studies and wondering, ‘Why is tenofovir not protecting these
women?’” Salim said. “It’s not protecting them because they’ve got Gardnerella,
and the Gardnerella is eating up all the tenofovir!”
tenofovir is an integral part of PrEP, or pre-exposure prophylaxis, a pill the
South African government has made available for free to sex workers and some
university students. Since the pill doesn’t travel through the
genital tract, PrEP might avoid being eroded by the vaginal microbiome, but the
Abdool Karims and their colleagues aren’t sure yet.
plenty of other evidence, however, that maintaining a healthy, Lactobacillus-dominant
vaginal microbiome protects against HIV. One meta-analysis of 23 studies from 2008
found bacterial vaginosis was associated with a 60 percent higher risk of HIV
infection. Just last month,
the researchers at AHRI found an extraordinarily high rate of bacterial
vaginosis—42 percent—among women in the region around Mtubatuba, where HIV is
also widespread.
scientists at CAPRISA and elsewhere are studying what exactly causes Prevotella
and Gardnerella to take over the vagina; they have found interesting
associations, but no common thread. Women with high levels of Prevotella in
their vaginas are more likely to be
obese, and black and Hispanic women, regardless of nationality, are
more likely to experience bacterial vaginosis. European women are more likely
to have Lactobacillus-dominant vaginas than African women are. (Could this be
why there’s so much more HIV in Africa than in Europe? Researchers don’t know.)
too, has a microbiome, and it’s even less studied than its vaginal counterpart.
But semen could be causing some of these vaginal disturbances: Semen contains
lots of foreign proteins, and women’s bodies become accustomed to those in
their regular partner’s semen. But if they are exposed to different proteins,
say those in their sugar daddy’s semen, “your body reacts like crazy,” Salim
says.
Depo-Provera shot is the most common form of birth control among poor women
here—largely because it’s convenient, and because women with unsupportive
partners can hide it from them. The problem, according to the CAPRISA
scientists, is that Depo contains high amounts of progestin, which tamps down
the levels of estrogen in the body. Because Lactobacillus flourishes in highly
estrogenic environments, Depo may open the door to Prevotella and other “bad”
bacteria.
most damaging to the vaginal microbiome are the practices women use to please
their blessers—or even just especially valuable boyfriends. A desirable vagina,
many women here believe, is tight and dry. It’s common for women to coax their
nether regions into this state by stuffing them with various powders, ashes,
and even chewing tobacco.
published in
2011 found that women who used “powders, creams, herbs, tablets,
sticks, stones, leaves, and traditional products” to dry out or tighten their
vaginas were 31 percent more likely to contract HIV. CAPRISA is now conducting
a study to see if the increased risk is due to inflammation, vaginal-bacteria
disturbances, or both.
 |
|
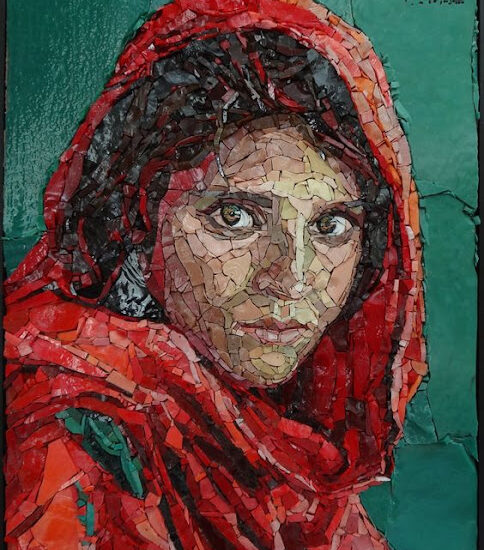
Mbali N.,
left, who once had a blesser, walks with a friend on a path in Vulindlela.
(Khaya Ngwenya / The Atlantic)
|
left CAPRISA, I met with another of its researchers, Sinaye Ngcapu, whose
colleagues call him Dr. Healthy Vagina. While Salim and Quarraisha guide all
the different facets of CAPRISA’s work, Ngcapu strives to decode the vaginal
microbiomes of African women. His goal is to design better HIV-prevention
tools—ones that don’t melt away in microbes’ presence.
grabbed an empty can of Coke Zero on the table to demonstrate why it’s
important to understand the microbiome if you want to stop HIV. “If you were to
understand how this Coca-Cola is made, you will know how to get rid of the
sugar that’s inside it,” he explained.
to ask Ngcapu whether his enthusiasm for the vaginal microbiome ever raises
eyebrows—at least among those outside the medical community.
black, young, and a member of another South African ethnic group, the Xhosa,
who live mainly in the country’s south. HIV tore through Xhosa communities,
too, and until very recently, apartheid kept people like Ngcapu from acquiring
the skills necessary to halt that devastation. To him, this battle is personal.
scary when you hear that in certain areas, one out of three women is positive,”
he said. “As a South African, you have to use South African strategies to
answer South African questions. If there will be a cure, it should come here,
where HIV is killing our brothers and sisters.”