Vaccines Alone Won’t Beat Ebola
Ed Yong,
The Atlantic, May 24, 2018
A deep
understanding of the Congo’s culture and time-honored public-health tactics are
the keys to controlling the outbreak.
understanding of the Congo’s culture and time-honored public-health tactics are
the keys to controlling the outbreak.
 |
|
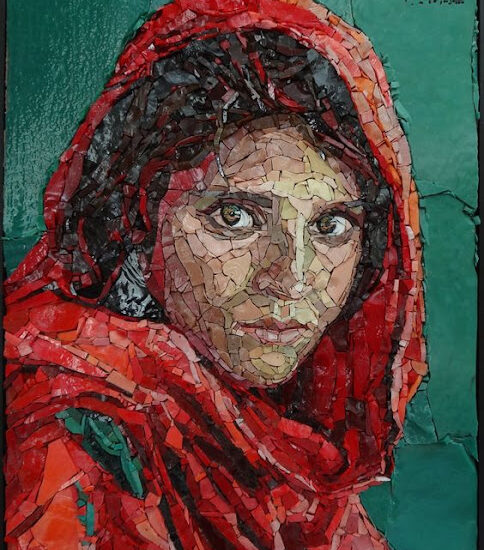
Kenny-Katombe
Butunka / Reuters |
Three
people who had been infected with Ebola recently left an
isolation ward at Wangata Hospital against medical advice, according
to the Democratic Republic of the Congo’s Ministry of Health. The hospital lies
in Mbandaka, a city of 1.2 million, where health workers are trying to contain
the Congo’s ninth Ebola outbreak. One patient was on the mend, but decided to
leave on Sunday and didn’t come back. Two more left with their families on
Monday and went to church. One died at home, before his body was returned to
the hospital for safe burial. The other returned voluntarily, before passing
away at the hospital.
people who had been infected with Ebola recently left an
isolation ward at Wangata Hospital against medical advice, according
to the Democratic Republic of the Congo’s Ministry of Health. The hospital lies
in Mbandaka, a city of 1.2 million, where health workers are trying to contain
the Congo’s ninth Ebola outbreak. One patient was on the mend, but decided to
leave on Sunday and didn’t come back. Two more left with their families on
Monday and went to church. One died at home, before his body was returned to
the hospital for safe burial. The other returned voluntarily, before passing
away at the hospital.
Choices
like these make it harder to control this outbreak, which had already spread to
58 possible cases, as of Wednesday evening. But they are also understandable.
like these make it harder to control this outbreak, which had already spread to
58 possible cases, as of Wednesday evening. But they are also understandable.
On a
recent trip to the Congo, I met several survivors of past Ebola outbreaks,
several of which had left hospitals and gone home. Partly, that’s because an
isolation ward can be a horrendous place, with walls and floors sometimes
covered with vomit, feces, and urine. But partly, it’s also because the very
concept of an isolation ward is an anathema to many Congolese people.
recent trip to the Congo, I met several survivors of past Ebola outbreaks,
several of which had left hospitals and gone home. Partly, that’s because an
isolation ward can be a horrendous place, with walls and floors sometimes
covered with vomit, feces, and urine. But partly, it’s also because the very
concept of an isolation ward is an anathema to many Congolese people.
In the
Congo, if you’re sick, you’re usually surrounded. Medical services are thin, so
family members shoulder the burden of nursing their loved ones back to health.
At one hospital I visited (well before the current outbreak), a family had camped
outside a treatment building, waiting for their relatives inside to recuperate.
Their laundry was drying on a washing line. “In an outbreak, you want to
separate sick and healthy people, but here, if people are sick, everyone’s
there,” one survivor told me. “Here, for we who live in communities, it is
solitude that kills us.”
Congo, if you’re sick, you’re usually surrounded. Medical services are thin, so
family members shoulder the burden of nursing their loved ones back to health.
At one hospital I visited (well before the current outbreak), a family had camped
outside a treatment building, waiting for their relatives inside to recuperate.
Their laundry was drying on a washing line. “In an outbreak, you want to
separate sick and healthy people, but here, if people are sick, everyone’s
there,” one survivor told me. “Here, for we who live in communities, it is
solitude that kills us.”
That
mindset continues after death. Families will clean and dress the bodies of
their loved ones. They’ll caress, kiss, and embrace them. Spouses might even
spend a night next to their deceased partners. Through these bonds of
affection, Ebola, which spreads through bodily fluids, can easily jump from one
host into an entire family. The worst thing about the virus is not its deeply
exaggerated bloodiness, but its ability to corrupt the bonds of community. It
is a pathogen well-suited to a world where sickness and death are met with
touch and affection.
mindset continues after death. Families will clean and dress the bodies of
their loved ones. They’ll caress, kiss, and embrace them. Spouses might even
spend a night next to their deceased partners. Through these bonds of
affection, Ebola, which spreads through bodily fluids, can easily jump from one
host into an entire family. The worst thing about the virus is not its deeply
exaggerated bloodiness, but its ability to corrupt the bonds of community. It
is a pathogen well-suited to a world where sickness and death are met with
touch and affection.
To bill
these choices and practices, and others like them, as superstitions
is misguided. These are the result of deeply held religious and cultural
beliefs. “If you’re asking someone to not do the typical thing they do to
grieve and mourn, you need to provide an appropriate alternative that achieves
the same cultural end,” says Maimuna Majumder, an epidemiologist at MIT.
“That’s usually the piece that goes missing. You can’t do that if you’re
othering these kinds of practices.”
these choices and practices, and others like them, as superstitions
is misguided. These are the result of deeply held religious and cultural
beliefs. “If you’re asking someone to not do the typical thing they do to
grieve and mourn, you need to provide an appropriate alternative that achieves
the same cultural end,” says Maimuna Majumder, an epidemiologist at MIT.
“That’s usually the piece that goes missing. You can’t do that if you’re
othering these kinds of practices.”
Fortunately,
the Ministry of Health understands that.“We can’t forcibly prevent family
members from touching a [patient],” says the spokesperson Jessica Ilunga. “So
we’ve been really stepping up our community-engagement activities, by involving
traditional and religious leaders. They have a huge influence on the
community.”
the Ministry of Health understands that.“We can’t forcibly prevent family
members from touching a [patient],” says the spokesperson Jessica Ilunga. “So
we’ve been really stepping up our community-engagement activities, by involving
traditional and religious leaders. They have a huge influence on the
community.”
That is
how outbreaks are contained—without community buy-in, resources and fancy new
technology won’t be enough. Unlike most of the Congo’s previous outbreaks,
mobile laboratories are now operating, allowing researchers to confirm possible
cases faster. As I reported on Monday, accurate
digital maps are being made. Tablets with freely
available software allow field workers to enter and compare data in
real time without having to rely on printed paper. And most excitingly, health
workers are starting to deploy an experimental vaccine called rVSV-ZEBOV.
how outbreaks are contained—without community buy-in, resources and fancy new
technology won’t be enough. Unlike most of the Congo’s previous outbreaks,
mobile laboratories are now operating, allowing researchers to confirm possible
cases faster. As I reported on Monday, accurate
digital maps are being made. Tablets with freely
available software allow field workers to enter and compare data in
real time without having to rely on printed paper. And most excitingly, health
workers are starting to deploy an experimental vaccine called rVSV-ZEBOV.
The
vaccine has been lauded as a “game changer”—and
rightly so. In over 40 years of Ebola outbreaks, never has such a tool been
available from the start. But it is still understudied in the field, and its
existence doesn’t guarantee victory against the outbreak. A recent New
York Times editorial, which somehow managed to describe a crisis
whose case numbers are still growing as “contained,” also billed the vaccine’s
use as “the first time Ebola was met with more than just the crude tools of
quarantine and hospice care.”
vaccine has been lauded as a “game changer”—and
rightly so. In over 40 years of Ebola outbreaks, never has such a tool been
available from the start. But it is still understudied in the field, and its
existence doesn’t guarantee victory against the outbreak. A recent New
York Times editorial, which somehow managed to describe a crisis
whose case numbers are still growing as “contained,” also billed the vaccine’s
use as “the first time Ebola was met with more than just the crude tools of
quarantine and hospice care.”
“Of
course you want vaccines, but yellow fever and cholera are perfect examples of
disease where we have vaccines and still get raging outbreaks,” says Nahid
Bhadelia, a physician at Boston University who helped to tackle
Ebola in Sierra Leone. “We still need the public-health pillars.”
course you want vaccines, but yellow fever and cholera are perfect examples of
disease where we have vaccines and still get raging outbreaks,” says Nahid
Bhadelia, a physician at Boston University who helped to tackle
Ebola in Sierra Leone. “We still need the public-health pillars.”
By that
she means: finding infected people and tracking their contacts; ensuring
hygienic practices that keep infections from spreading; and engaging with
communities. These are old-school measures. Public Health 101. But they’re also
the bedrock of any outbreak response. They’re vital for diseases that have no
available vaccines or treatments, like Lassa fever
which is currently breaking out in Liberia, or Nipah
which has risen again in India. And they’re still vital when vaccines are
available.
she means: finding infected people and tracking their contacts; ensuring
hygienic practices that keep infections from spreading; and engaging with
communities. These are old-school measures. Public Health 101. But they’re also
the bedrock of any outbreak response. They’re vital for diseases that have no
available vaccines or treatments, like Lassa fever
which is currently breaking out in Liberia, or Nipah
which has risen again in India. And they’re still vital when vaccines are
available.
Around
7,500 doses of vaccine have so far been sent to the Congo, and 73 have been
used as of Thursday afternoon, according to Guillaume Ngoie Mwamba. He is
leading the DRC’s vaccination program and, to show people that the vaccine is
safe, was the first to get the shot.
7,500 doses of vaccine have so far been sent to the Congo, and 73 have been
used as of Thursday afternoon, according to Guillaume Ngoie Mwamba. He is
leading the DRC’s vaccination program and, to show people that the vaccine is
safe, was the first to get the shot.
The plan
is to start by immunizing health workers, people who have come into contact
with confirmed patients, and contacts of those contacts. This “ring
vaccination” strategy entirely depends on basic public health. Without a full
list of contacts, the rings will be broken and the Ebola will slip out. “If you
don’t know the chain, who do you vaccinate?” says Seth Berkley of Gavi, a
nonprofit that has supported the
vaccination campaign. That’s why the vaccine has thus far only been
used in Mbandaka. It has taken longer to flesh out the contact lists in rural
Bikoro and Iboko, where most cases have occurred, although Mwamba expects
vaccination to begin there on Saturday.
is to start by immunizing health workers, people who have come into contact
with confirmed patients, and contacts of those contacts. This “ring
vaccination” strategy entirely depends on basic public health. Without a full
list of contacts, the rings will be broken and the Ebola will slip out. “If you
don’t know the chain, who do you vaccinate?” says Seth Berkley of Gavi, a
nonprofit that has supported the
vaccination campaign. That’s why the vaccine has thus far only been
used in Mbandaka. It has taken longer to flesh out the contact lists in rural
Bikoro and Iboko, where most cases have occurred, although Mwamba expects
vaccination to begin there on Saturday.
Even with
complete lists, there’s a lot of work to do. The Ministry of Health noted yesterday
that some people from Bikoro were refusing to cooperate with health workers. To
address that, Raoul Kamanda, a communications director from the Ministry of
Health, held a meeting with a Bikoro citizens’ association to draw up plans for
better communicating with the community.
complete lists, there’s a lot of work to do. The Ministry of Health noted yesterday
that some people from Bikoro were refusing to cooperate with health workers. To
address that, Raoul Kamanda, a communications director from the Ministry of
Health, held a meeting with a Bikoro citizens’ association to draw up plans for
better communicating with the community.
For a
start, there’s a language barrier. The Congo has upward of 200 languages. In
Bikoro, around 90 percent of people speak Lingala, the main local dialect; to
reach the people who don’t, the ministry is also translating its messages into
N’Tomba, which is spoken by 40 percent of the region.
start, there’s a language barrier. The Congo has upward of 200 languages. In
Bikoro, around 90 percent of people speak Lingala, the main local dialect; to
reach the people who don’t, the ministry is also translating its messages into
N’Tomba, which is spoken by 40 percent of the region.
This kind
of outreach must precede the deployment of the rVSV-ZEBOV vaccine, which brings
with it several complications. Berkley says that people in the affected
province are used to vaccination campaigns where entire communities get shots
for diseases like measles or tetanus. But there aren’t enough doses of the
Ebola vaccine for that. The ring-vaccination strategy, where only certain
people get immunized, is a trickier concept to convey.
of outreach must precede the deployment of the rVSV-ZEBOV vaccine, which brings
with it several complications. Berkley says that people in the affected
province are used to vaccination campaigns where entire communities get shots
for diseases like measles or tetanus. But there aren’t enough doses of the
Ebola vaccine for that. The ring-vaccination strategy, where only certain
people get immunized, is a trickier concept to convey.
Since the
vaccine hasn’t yet been licensed, it is being rolled out as part of a clinical
trial, which means that every recipient must give informed consent. In a similar
small trial in Guinea, rVSV-ZEBOV proved to be 100 percent effective
at preventing Ebola infections, but only during the tail end of an outbreak.
It’s unlikely to offer perfect protection in a more realistic setting, so it’s
vital that vaccinated people don’t let their guard down. The vaccine also takes
10 days to provide full protection; it has only been 16 days since the new
Congo outbreak was first declared.
vaccine hasn’t yet been licensed, it is being rolled out as part of a clinical
trial, which means that every recipient must give informed consent. In a similar
small trial in Guinea, rVSV-ZEBOV proved to be 100 percent effective
at preventing Ebola infections, but only during the tail end of an outbreak.
It’s unlikely to offer perfect protection in a more realistic setting, so it’s
vital that vaccinated people don’t let their guard down. The vaccine also takes
10 days to provide full protection; it has only been 16 days since the new
Congo outbreak was first declared.
“If you
say to people that it’s 100 percent effective, and all contacts get vaccinated,
some subset of them will develop Ebola because they’ve already been incubating
the virus,” says Berkley. “We have to be careful to not lose confidence in the
vaccine.”
say to people that it’s 100 percent effective, and all contacts get vaccinated,
some subset of them will develop Ebola because they’ve already been incubating
the virus,” says Berkley. “We have to be careful to not lose confidence in the
vaccine.”
These
challenges are not insurmountable. Mwamba tells me that there was originally
some resistance to the vaccine among people in Mbandaka but after speaking to
the communications team, everyone who was approached agreed to get the shot.
challenges are not insurmountable. Mwamba tells me that there was originally
some resistance to the vaccine among people in Mbandaka but after speaking to
the communications team, everyone who was approached agreed to get the shot.
Reassuringly,
a team of experts from Guinea, who were all involved in the rVSV-ZEBOV
vaccination trial from 2015, arrived in
Mbandaka on Sunday. They are intimately familiar with Ebola, ring
vaccination, and this particular vaccine. “They’ve very important,” says
Mwanba. “They’re training the Congolese, and I think by the end of this
outbreak, we’ll have enough capacity to fight new epidemics on our own when
they come again.” So far, the vaccination team includes six of the Guineans,
along with 18 Congolese health workers. More people from Mbandaka and Bikoro
are also being recruited to enhance local knowledge.
a team of experts from Guinea, who were all involved in the rVSV-ZEBOV
vaccination trial from 2015, arrived in
Mbandaka on Sunday. They are intimately familiar with Ebola, ring
vaccination, and this particular vaccine. “They’ve very important,” says
Mwanba. “They’re training the Congolese, and I think by the end of this
outbreak, we’ll have enough capacity to fight new epidemics on our own when
they come again.” So far, the vaccination team includes six of the Guineans,
along with 18 Congolese health workers. More people from Mbandaka and Bikoro
are also being recruited to enhance local knowledge.
This
vaccine may well help beat Ebola. But even if it does, its success will have
been predicated on “crude tools”—on tracing contacts, on speaking a shared
language, on cultural understanding, on trust. “It’s not surprising that people
often don’t see how important these measures are,” says Majumder. “In public
health, when you do your job right, no one knows that you do it.”
vaccine may well help beat Ebola. But even if it does, its success will have
been predicated on “crude tools”—on tracing contacts, on speaking a shared
language, on cultural understanding, on trust. “It’s not surprising that people
often don’t see how important these measures are,” says Majumder. “In public
health, when you do your job right, no one knows that you do it.”