Traumatic brain injury: The unseen impact of domestic violence
Paul van
Donkelaar, The Conversaion, April 16, 2018
The last
time Susan’s husband lost his temper, he smashed her head against the kitchen
wall so many times she lost count before she managed to flee with just the
clothes on her back and some basic identification.
time Susan’s husband lost his temper, he smashed her head against the kitchen
wall so many times she lost count before she managed to flee with just the
clothes on her back and some basic identification.
 |
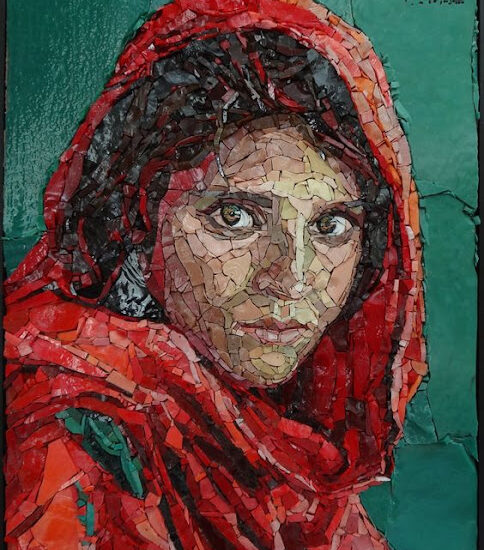
| One third of women will suffer violence at the hands of someone they love, sometimes resulting in traumatic brain injury. Here, women lay on the street to protest this violence, in Pamplona in northern Spain, in 2015. (AP Photo/Alvaro Barrientos) |
At the
local women’s shelter where she ended up, Susan was expected to accomplish a
lot during a maximum 30-day stay: Attend counselling, secure employment or
social assistance, meet with a lawyer and find permanent housing.
local women’s shelter where she ended up, Susan was expected to accomplish a
lot during a maximum 30-day stay: Attend counselling, secure employment or
social assistance, meet with a lawyer and find permanent housing.
Women
like Susan are on the radar in British Columbia right now as April 15-21 marks
Prevention of Violence Against Women Week in the province.
like Susan are on the radar in British Columbia right now as April 15-21 marks
Prevention of Violence Against Women Week in the province.
The
statistics are terrifying: In Canada, one woman is
killed every week by her partner; globally, one third of
women will suffer violence at the hands of someone they love in their lifetime.
statistics are terrifying: In Canada, one woman is
killed every week by her partner; globally, one third of
women will suffer violence at the hands of someone they love in their lifetime.
But what
if survivors like Susan are also dealing with the effects
of a traumatic brain injury along with the fear and trauma of
finally having escaped a long-term abusive relationship?
if survivors like Susan are also dealing with the effects
of a traumatic brain injury along with the fear and trauma of
finally having escaped a long-term abusive relationship?
As a
neuroscientist and professor at the University of British Columbia with
expertise in traumatic brain injury, I know the impacts of this injury can be
devastating — ranging from headaches, double vision and nausea to difficulty
concentrating, remembering things and completing simple tasks.
neuroscientist and professor at the University of British Columbia with
expertise in traumatic brain injury, I know the impacts of this injury can be
devastating — ranging from headaches, double vision and nausea to difficulty
concentrating, remembering things and completing simple tasks.
It’s also
clear the effects tend to be worse when the trauma occurs repeatedly over time,
with symptoms lasting for months to years.
clear the effects tend to be worse when the trauma occurs repeatedly over time,
with symptoms lasting for months to years.
Victims
hesitant to seek help
hesitant to seek help
Much of
what we know about traumatic brain injury is the result of a large body of
research and media attention over the last 10 to 15 years on athletes and
sports-related concussion.
what we know about traumatic brain injury is the result of a large body of
research and media attention over the last 10 to 15 years on athletes and
sports-related concussion.
Until
recently, the link between traumatic brain injury and intimate partner violence
has been largely unexplored.
recently, the link between traumatic brain injury and intimate partner violence
has been largely unexplored.
So, since
June of 2017, my research team has been collaborating with Kelowna Women’s Shelter in
a community-based research project designed to examine the connection between
traumatic brain injury and intimate partner violence.
June of 2017, my research team has been collaborating with Kelowna Women’s Shelter in
a community-based research project designed to examine the connection between
traumatic brain injury and intimate partner violence.
Researching
this population can be challenging. Victims are often hesitant to seek help
because of the stigma associated with intimate partner violence.
this population can be challenging. Victims are often hesitant to seek help
because of the stigma associated with intimate partner violence.
This can
lead to a survivor, seemingly paradoxically, returning to
their abuser repeatedly over the course of months or years, thereby
increasing the likelihood of multiple head injuries and chronic symptoms.
lead to a survivor, seemingly paradoxically, returning to
their abuser repeatedly over the course of months or years, thereby
increasing the likelihood of multiple head injuries and chronic symptoms.
Unlike
athletes who have suffered a sport-related concussion, survivors of intimate
partner violence also quite often experience emotional difficulties such as
post-traumatic stress disorder (PTSD), depression and anxiety.
athletes who have suffered a sport-related concussion, survivors of intimate
partner violence also quite often experience emotional difficulties such as
post-traumatic stress disorder (PTSD), depression and anxiety.
Despite
these challenges, an increasing number of researchers have recently started to
examine traumatic brain injury in this vulnerable population. Part of the
motivation for doing so is the large number of women thought to be affected.
these challenges, an increasing number of researchers have recently started to
examine traumatic brain injury in this vulnerable population. Part of the
motivation for doing so is the large number of women thought to be affected.
In
particular, the U.S.
Centers for Disease Control and Prevention reports, each year, 2.3
per cent of women over the age of 18 experience severe physical violence
including “being slammed against something” or “being hit with a fist or
something hard.”
particular, the U.S.
Centers for Disease Control and Prevention reports, each year, 2.3
per cent of women over the age of 18 experience severe physical violence
including “being slammed against something” or “being hit with a fist or
something hard.”
Furthermore,
up to 90 per cent
of survivors of intimate partner violence report head, neck and face injuries
at least once and typically on multiple occasions.
up to 90 per cent
of survivors of intimate partner violence report head, neck and face injuries
at least once and typically on multiple occasions.
Assuming
similar percentages in Canada, this translates into approximately 276,000 women
per year who will suffer a traumatic brain injury as a result of intimate
partner violence.
similar percentages in Canada, this translates into approximately 276,000 women
per year who will suffer a traumatic brain injury as a result of intimate
partner violence.
Memory
and learning challenges
and learning challenges
Research
with this population to date shows survivors of intimate partner
violence who suffer a traumatic brain injury report symptoms such as
headache, difficulty sleeping and cognitive deficits consistent with the head
injury.
with this population to date shows survivors of intimate partner
violence who suffer a traumatic brain injury report symptoms such as
headache, difficulty sleeping and cognitive deficits consistent with the head
injury.
In terms
of brain function, it has been demonstrated the more severe the reported
traumatic brain injuries in this population the larger the deficits in memory
and learning. These deficits, in turn, are related to alterations in how different circuits
in the brain communicate with each other.
of brain function, it has been demonstrated the more severe the reported
traumatic brain injuries in this population the larger the deficits in memory
and learning. These deficits, in turn, are related to alterations in how different circuits
in the brain communicate with each other.
Our
research explores both the emotional and physiological disturbances which occur
in women who have survived intimate partner violence, in order to develop a
deeper understanding of this issue.
research explores both the emotional and physiological disturbances which occur
in women who have survived intimate partner violence, in order to develop a
deeper understanding of this issue.
In one
part of the study participants complete questionnaires assessing PTSD,
depression and anxiety.
part of the study participants complete questionnaires assessing PTSD,
depression and anxiety.
In a
second part, we carry out cerebrovascular and sensorimotor assessments along
with blood draws
to assess for levels of various markers of brain injury.
second part, we carry out cerebrovascular and sensorimotor assessments along
with blood draws
to assess for levels of various markers of brain injury.
Changing
the conversation
the conversation
So what
does all this science mean for Susan and women like her? In addition to
gathering more data on the incidence of traumatic brain injury in this
population, our project aims to improve the lives of victims and those who
support them.
does all this science mean for Susan and women like her? In addition to
gathering more data on the incidence of traumatic brain injury in this
population, our project aims to improve the lives of victims and those who
support them.
The fact
is, staff at women’s shelters and many other women serving agencies generally
don’t have the knowledge, training or tools to screen for brain injury at
intake.
is, staff at women’s shelters and many other women serving agencies generally
don’t have the knowledge, training or tools to screen for brain injury at
intake.
This
means many clients who have suffered a traumatic brain injury are not getting
the support they really need to accomplish their goals and move forward into a
life free of abuse.
means many clients who have suffered a traumatic brain injury are not getting
the support they really need to accomplish their goals and move forward into a
life free of abuse.
We hope
our research will help change the conversation around traumatic brain injury in
this population, as it has for athletes, and shine a spotlight on the
unacceptable problem of traumatic brain injury in women at the hands of the
ones they love.
our research will help change the conversation around traumatic brain injury in
this population, as it has for athletes, and shine a spotlight on the
unacceptable problem of traumatic brain injury in women at the hands of the
ones they love.