More than one in 100 Nunavut infants have TB
Sarah
Giles, The Conversation, April 8, 2018
Canada’s
simmering tuberculosis (TB) outbreak in northern communities is likely much
worse than suspected.
simmering tuberculosis (TB) outbreak in northern communities is likely much
worse than suspected.
 |
|
Tuberculosis
has been a problem for decades among Canada’s northern
Indigenous population.
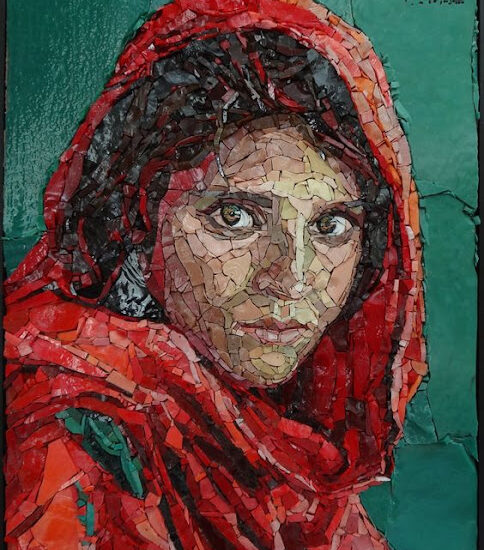
New data obtained through access to information requests
reveals shockingly
high TB rates among Nunavut’s infants. Poor data collection
indicates the real
rates will be even higher. (Gar Lunney/Library and Archives Canada) |
A report newly obtained through an
access-to-information (ATI) request reveals that the incidence rate
of TB among Nunavut’s infants (under one year of age) was 1,020 cases per
100,000 people in 2017 — a shockingly high level.
access-to-information (ATI) request reveals that the incidence rate
of TB among Nunavut’s infants (under one year of age) was 1,020 cases per
100,000 people in 2017 — a shockingly high level.
In the
rest of Canada, the rate is just three infants
per 100,000.
rest of Canada, the rate is just three infants
per 100,000.
Worse,
the actual rate may be higher than the report indicates, as it drew only on
data from the first nine months of 2017. An additional 21 cases of TB (in
people of unknown ages) were identified before the year ended. Many important
data points were never collected.
the actual rate may be higher than the report indicates, as it drew only on
data from the first nine months of 2017. An additional 21 cases of TB (in
people of unknown ages) were identified before the year ended. Many important
data points were never collected.
Despite
these concerning numbers, Minister of Health Ginette Petipas Taylor, Minister
of Indigenous Services Jane Philpott and Inuit Tapiriit Kanatami (ITK)
president Natan Obed recently announced the ambitious goal of eliminating TB
from Canada’s North by 2030.
these concerning numbers, Minister of Health Ginette Petipas Taylor, Minister
of Indigenous Services Jane Philpott and Inuit Tapiriit Kanatami (ITK)
president Natan Obed recently announced the ambitious goal of eliminating TB
from Canada’s North by 2030.
While it
is commendable to see political will and $27.5 million
over five years supporting TB elimination, similar
announcements for TB reduction were made by federal ministers of health in 1997
and 2006. These targets were not met.
is commendable to see political will and $27.5 million
over five years supporting TB elimination, similar
announcements for TB reduction were made by federal ministers of health in 1997
and 2006. These targets were not met.
The main
hope arising from the latest plan is that ITK, a
non-profit organization advancing the rights and interests of Inuit in Canada,
is leading the process for the first time.
hope arising from the latest plan is that ITK, a
non-profit organization advancing the rights and interests of Inuit in Canada,
is leading the process for the first time.
Hard to
diagnose in babies
diagnose in babies
I work as
a family and emergency room doctor in the Northwest Territories. I also have a
diploma in tropical medicine and hygiene and I do work with Doctors without Borders.
a family and emergency room doctor in the Northwest Territories. I also have a
diploma in tropical medicine and hygiene and I do work with Doctors without Borders.
I have
seen the devastation that TB reaps. I am concerned by the high incidence rate
of TB in Nunavut’s babies. The poor data we have indicate that TB is a bigger
problem than the current numbers reveal.
seen the devastation that TB reaps. I am concerned by the high incidence rate
of TB in Nunavut’s babies. The poor data we have indicate that TB is a bigger
problem than the current numbers reveal.
Eliminating
TB in the North in just 12 years may be harder than many imagine.
TB in the North in just 12 years may be harder than many imagine.
 |
|
Inuit
Tapiriit Kanatami (ITK) President Natan Obed addresses media in Ottawa
on
Oct.5, 2017, while Indigenous Services Minister Jane Philpott (left) and Health Minister Ginette Petitpas Taylor (centre) look on. THE CANADIAN PRESS/Sean Kilpatrick |
While
most people think of TB as a bacterial disease of the lungs found in
resource-poor countries, it can also present virtually anywhere in the body,
especially in infants.
most people think of TB as a bacterial disease of the lungs found in
resource-poor countries, it can also present virtually anywhere in the body,
especially in infants.
TB is
particularly hard to
diagnose in babies because the symptoms — of poor
weight gain, lack of playfulness and fever — are not very specific.
particularly hard to
diagnose in babies because the symptoms — of poor
weight gain, lack of playfulness and fever — are not very specific.
In
general, only affluent countries with excellent health care can definitely
diagnose babies through technical and expensive tests and, even then, many
cases are missed.
general, only affluent countries with excellent health care can definitely
diagnose babies through technical and expensive tests and, even then, many
cases are missed.
It is
difficult to know the true extent of tuberculosis in babies throughout the
world, but it is patently unacceptable for one in 100 babies in Nunavut to have
active TB.
difficult to know the true extent of tuberculosis in babies throughout the
world, but it is patently unacceptable for one in 100 babies in Nunavut to have
active TB.
A legacy
of fear and stigma
of fear and stigma
Tuberculosis
has been present in the area now known as Nunavut for more than 100
years but it has not always been so prevalent. As recently as 1997,
the incidence was 31 cases per
100,000.
has been present in the area now known as Nunavut for more than 100
years but it has not always been so prevalent. As recently as 1997,
the incidence was 31 cases per
100,000.
TB has
once again become an everyday reality for the people of Nunavut — due to the
Public Health Agency of Canada’s premature
closure of TB control programs like the Canadian Tuberculosis
Committee and its Aboriginal Scientific Tuberculosis Subcommittee in 2011, the
dramatic under-funding
of Indigenous health care, poor social
determinants of health and a lack of human
resources in the health-care field.
once again become an everyday reality for the people of Nunavut — due to the
Public Health Agency of Canada’s premature
closure of TB control programs like the Canadian Tuberculosis
Committee and its Aboriginal Scientific Tuberculosis Subcommittee in 2011, the
dramatic under-funding
of Indigenous health care, poor social
determinants of health and a lack of human
resources in the health-care field.
The
historical context of the treatment of Inuit with suspected TB cannot be
understated. During the
1940s through the 1960s, thousands of Inuit people thought to have TB were taken
from their villages and sent to sanitoriums in places like Hamilton, Ont.
historical context of the treatment of Inuit with suspected TB cannot be
understated. During the
1940s through the 1960s, thousands of Inuit people thought to have TB were taken
from their villages and sent to sanitoriums in places like Hamilton, Ont.
Most
never had a chance to say goodbye to their families and many never returned.
never had a chance to say goodbye to their families and many never returned.
A legacy
of fear and the
stigma of a communicable disease in small towns continues to deter
people from seeking medical help today.
of fear and the
stigma of a communicable disease in small towns continues to deter
people from seeking medical help today.
Lifelong
cognitive impairment
cognitive impairment
A person
exposed to Mycobacterium tuberculosis bacteria will usually not develop the
disease. Some, however, will only
partially fight off infection and will develop latent TB. Of those
with latent TB, five to 10 per cent will go on to develop symptoms of the disease,
or active TB.
exposed to Mycobacterium tuberculosis bacteria will usually not develop the
disease. Some, however, will only
partially fight off infection and will develop latent TB. Of those
with latent TB, five to 10 per cent will go on to develop symptoms of the disease,
or active TB.
Those with weakened
immune systems and babies are at heightened risk of developing
active TB.
immune systems and babies are at heightened risk of developing
active TB.
Active TB
is a potentially deadly infection and, if in the lungs, is contagious. People
exposed to the disease can receive preventative treatment to decrease their
risk of developing it.
is a potentially deadly infection and, if in the lungs, is contagious. People
exposed to the disease can receive preventative treatment to decrease their
risk of developing it.
Though
infants in Nunavut receive a TB vaccine at
birth, it is not entirely
protective.
infants in Nunavut receive a TB vaccine at
birth, it is not entirely
protective.
The high
incidence rate of TB among Nunavut’s infants is especially worrisome given that
Nunavut has the highest
fertility rate in the country, with women giving birth to an average
of 2.9 children, compared to the Canadian average of 1.6 children.
incidence rate of TB among Nunavut’s infants is especially worrisome given that
Nunavut has the highest
fertility rate in the country, with women giving birth to an average
of 2.9 children, compared to the Canadian average of 1.6 children.
This
means many more infants are in danger.
means many more infants are in danger.
 |
|
A group
of young Inuit children play in Gjoa Haven, Nunavut in August 2013.
THE
CANADIAN PRESS/Sean Kilpatrick |
While
Nunavut did not report any infant deaths in 2017, the consequences of even a
successfully treated TB infection can include a host of problems, including lifelong
cognitive impairment.
Nunavut did not report any infant deaths in 2017, the consequences of even a
successfully treated TB infection can include a host of problems, including lifelong
cognitive impairment.
Since
babies exposed to TB tend to develop active disease faster than adults, infant
TB is a sign that the disease is circulating
in the community.
babies exposed to TB tend to develop active disease faster than adults, infant
TB is a sign that the disease is circulating
in the community.
The true
crux of Nunavut’s TB problem, as shown by the documents I obtained through the
Public Health Agency of Canada (PHAC), is that poor data quality and a lack of
data showing preventative treatment measures means that nobody fully knows the
extent of the outbreak.
crux of Nunavut’s TB problem, as shown by the documents I obtained through the
Public Health Agency of Canada (PHAC), is that poor data quality and a lack of
data showing preventative treatment measures means that nobody fully knows the
extent of the outbreak.
TB
monitoring failures
monitoring failures
I sent
ATI requests to the Ministry of Health in Nunavut, Health Canada and PHAC
asking how many people in Nunavut were offered prophylactic treatment after
being exposed to TB, how many received it and how many completed it.
ATI requests to the Ministry of Health in Nunavut, Health Canada and PHAC
asking how many people in Nunavut were offered prophylactic treatment after
being exposed to TB, how many received it and how many completed it.
Ron
Wassink, a communications specialist for the Nunavut Department of Health. said
that no statistics for prophylactic treatment are available because: “The
database is still under development and as such is not ready to create summary
statistics nor would it be appropriate to do so at this time until the database
is fully operational.”
Wassink, a communications specialist for the Nunavut Department of Health. said
that no statistics for prophylactic treatment are available because: “The
database is still under development and as such is not ready to create summary
statistics nor would it be appropriate to do so at this time until the database
is fully operational.”
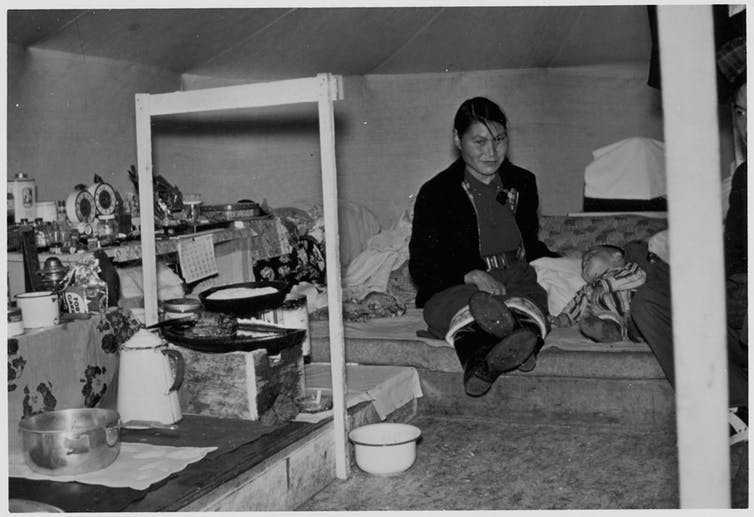 |
| At least one-third of Inuit were infected with TB in the 1950s. Here, an Inuit woman with active tuberculosis sits with her young son. (Health and Welfare Canada / Library and Archives Canada) |
Prophylactic
treatment can prevent people from developing latent TB, the not-yet-contagious
precursor to active TB. Knowing the number of people offered prophylactic
treatment, a treatment that is recommended by the World Health Organization but
is not mandatory, gives researchers a true grasp of the amount of disease
circulating in a community.
treatment can prevent people from developing latent TB, the not-yet-contagious
precursor to active TB. Knowing the number of people offered prophylactic
treatment, a treatment that is recommended by the World Health Organization but
is not mandatory, gives researchers a true grasp of the amount of disease
circulating in a community.
The data
that do exist about the outbreak, as shown in the PHAC report I accessed, are
frighteningly incomplete.
that do exist about the outbreak, as shown in the PHAC report I accessed, are
frighteningly incomplete.
The
report explains that each community in Nunavut should have been keeping a
separate Excel spreadsheet for active cases and contacts and importing them
into a database. However, some Nunavut communities were left out of this
process because their records were “in a format not conducive for data import.”
report explains that each community in Nunavut should have been keeping a
separate Excel spreadsheet for active cases and contacts and importing them
into a database. However, some Nunavut communities were left out of this
process because their records were “in a format not conducive for data import.”
Even now,
in 2018, there is no adequate database for TB monitoring.
in 2018, there is no adequate database for TB monitoring.
Incidence
rates out of control
rates out of control
Each
active case of TB requires contact investigation. This helps health officials
find people who are at risk of developing and spreading the disease.
active case of TB requires contact investigation. This helps health officials
find people who are at risk of developing and spreading the disease.
Contacts,
which include people living in the same house, should be offered prophylactic
treatment if they qualify for it, or they should receive follow-up monitoring
for two years to check for symptoms.
which include people living in the same house, should be offered prophylactic
treatment if they qualify for it, or they should receive follow-up monitoring
for two years to check for symptoms.
The
report shows that local health care workers failed to list the contact type in
42.4 per cent of investigations. This is assigned based on how much time the
patient spent with their family member, spouse or perhaps a friend staying in
their home.
report shows that local health care workers failed to list the contact type in
42.4 per cent of investigations. This is assigned based on how much time the
patient spent with their family member, spouse or perhaps a friend staying in
their home.
The
categorization of contact type is vital for determining whether a person should
be treated.
categorization of contact type is vital for determining whether a person should
be treated.
While the
federal government’s funding announcement and strategy are important steps in
the right direction, the PHAC report shows that the current data are of poor
quality and that the incidence rate of TB in Nunavut’s most vulnerable
population is out of control.
federal government’s funding announcement and strategy are important steps in
the right direction, the PHAC report shows that the current data are of poor
quality and that the incidence rate of TB in Nunavut’s most vulnerable
population is out of control.
With the
hiring of more staff, a more culturally sensitive program and better quality
data, it is entirely likely that the number of cases of TB detected will
actually increase before they decrease because of better detection.
hiring of more staff, a more culturally sensitive program and better quality
data, it is entirely likely that the number of cases of TB detected will
actually increase before they decrease because of better detection.
Until we
can accurately quantify the scope of the current problem, it is very difficult
to foresee an end to the current TB outbreak.
can accurately quantify the scope of the current problem, it is very difficult
to foresee an end to the current TB outbreak.